Every modern healthcare institution implements practices for infection prevention and control to ensure patient safety. A key strategy for managing the spread of infectious diseases is isolating patients with infections in airborne infection isolation rooms (AIIRs).
These rooms, designed for a single patient, confine the infected individual in a private area and use advanced ventilation systems to remove infectious aerosols from the surroundings. Research shows that the rooms are highly effective in preventing the spread of infectious diseases within a hospital.
Most infectious diseases are transmitted between people through direct contact, touching contaminated surfaces, or inhaling airborne droplets. When people with an infection cough or sneeze, they release respiratory droplets and aerosols carrying bacteria or viruses into the air. The airborne pathogens can then spread through the environment and settle on surfaces which are then known as fomites. Anyone who touches these surfaces or breathes air containing infected droplets or aerosols, is at a higher risk of contracting the disease. This includes patients, staff, and visitors in the affected area.
The Centers for Disease Control recommends specific precautions for treating patients potentially infected with contagious diseases. These include isolating them in AIIRs to prevent the spread of infection. Unlike general patient rooms, AIIRs are sealed using negative pressure that keeps air inside with controlled ventilation so that bacteria and viruses do not escape into the general areas of a hospital.
This technology keeps the air inside the room and ensures it does not mix with the air in general hospital areas. The air in AIIRs is controlled and filtered to prevent bacteria and viruses from escaping, reducing the threat of outbreaks.
These rooms are designed with several safety features. They have a secure entry system, doors that can be sealed tightly, and high-efficiency particulate air (HEPA) filters. These filters are similar to those used in cleanrooms and other environments requiring high air purity. HEPA filters play a crucial role in the ventilation system of AIIRs by removing airborne pathogens.
Additional safety measures in AIIRs include anterooms, along with strict hygiene and waste management protocols, further reducing the risk of airborne transmission of infections throughout the hospital.
The Evolution of AIIRs
The concept of isolation treatment has a long history, dating back to the late 1700s. It was initially implemented to separate individuals with contagious diseases such as typhoid, scarlet fever, smallpox, and the plague. During those times, the ill were isolated in specific sections of hospitals, homes, or epidemic houses. This practice continued as a crucial precautionary measure against disease transmission until the discovery of penicillin.
However, despite isolating patients with specific illnesses in designated hospital wards, outbreaks would frequently lead to the closure of these wards due to inadequate infection control measures.
Notably, shortcomings in infection control became evident during significant events like the 2001 U.S. anthrax crisis, the 2003 SARS (severe acute respiratory syndrome) pandemic, and the 2009 influenza H1N1 outbreak. In response to these challenges, the EUNID (European Network for Highly Infectious Diseases) undertook a six-year project aimed at improving high-level infection control. This initiative facilitated the exchange of information among leading clinicians and the sharing of best practices in the care of highly infectious disease patients.
Through extensive research and collaboration with medical experts, the use of high-level isolation units emerged as the most effective method for controlling high-level infections.
By 2014, 56 U.S. hospitals were equipped with high-level isolation units, specifically designed as airborne infection isolation rooms to care for patients with highly contagious diseases. Today, modern healthcare facilities incorporate dedicated airborne infectious isolation rooms as an integral part of their infection management and control strategies. According to the CDC, all acute-care inpatient facilities need at least one AIIR.
The Risk Posed by Airborne Pathogens
Communicable diseases are different from non-communicable ones like cancer, diabetes, and asthma because they can spread from one person to another through the exchange of pathogens like bacterial and viral microorganisms. Examples of communicable diseases include:
- COVID-19
- Chickenpox
- Mumps
- Measles
- Whooping cough
- Tuberculosis
- Diphtheria
- Pneumonia
As everyone learned from the COVID-19 outbreak, individuals can contract a communicable disease without even direct contact with an infected person. The tiny, aerosolized particles released by infected individuals can linger in the air for extended periods. These particles can either remain confined within rooms or travel significant distances on air currents before coming into contact with another person. For instance, the measles virus can remain airborne for up to two hours after an infected person has left a room.
Those who breathe in these particles are at a heightened risk of contracting the disease. Preventing airborne pathogen transmission in AIIRs requires specially designed ventilation systems equipped with effective filtration mechanisms. These controls are supplemented with infection prevention measures such as regular handwashing, thorough antiseptic cleaning, and the use of personalized protective equipment.
Guidelines for Air Handling in Isolation Rooms
The American Society of Heating, Refrigerating, and Air-Conditioning Engineers (ASHRAE) Standard 170 lays out specific requirements for selecting equipment when designing the mechanical systems for isolation rooms. Components include air handling systems to maintain the necessary differential air pressure between adjacent areas, regulate airflow, and incorporate air filtration.
According to the International Health Guidelines, HEPA filters are recommended for both supply and exhaust air in isolation rooms. Ideally, air from AIIRs should be directly exhausted to the outdoors.
HEPA filters are tested and certified to capture at a minimum of 99.7% at .03 microns, and they efficiently capture particles both larger and smaller than the most penetrating particle size (MPPS). Typically, the contaminated aerosols targeted for removal from an AIIR measure less than 5 µm in size. According to the CDC, HEPA filters exhibit even greater efficiency compared to filters with MERV 16 ratings when it comes to capturing smaller infectious particles generated by humans.
Filtration with High Air Exchange
AIIRs maintain high rates of air exchange for both air supply and exhaust flow rates compared to other sections of the hospital. According to CDC guidelines, isolation rooms should achieve a minimum of 12 air changes per hour (ACH). This ACH 12 rating signifies how many times the room’s air is completely exchanged with fresh air within an hour, effectively minimizing the risk of infectious disease transmission.
To calculate the ACH rate, you can use the following formula:
ACH = (CFM, which represents the airflow in cubic feet per minute) x 60 (minutes in an hour) / (cubic feet of the space, calculated by multiplying its length by width by the height of the ceiling).
For example, a room measuring 20 feet by 10 feet with a ceiling height of 10 feet, and an HVAC system with a supply air ventilation rate of 400 CFM, would achieve an ACH rating of 12. This means that the room’s air is completely replaced with fresh air 12 times every hour, ensuring a high level of cleanliness and reducing the risk of disease transmission.
The Importance of Filter Efficiency
When it comes to air purification, the function of all physical air filters is the same: as air passes through them, they capture particles of various sizes, including pathogens, allergens, and dust. There are a variety of filters available in the market, each possessing different efficiency ratings for capturing different types of particles of various sizes.
One common measurement used to gauge filter efficiency is the MERV (minimum efficiency reporting value) rating, which assesses a filter’s ability to trap particles ranging from 0.3 to 10 microns in size. This rating system is based on a testing method established by the American Society of Heating, Refrigeration, and Air Conditioning Engineers (ASHRAE). Filters are categorized on a scale from 1 to 16 based on their MERV ratings, with higher numbers indicating superior filtration capabilities.
This table outlines the efficiency of different filters in capturing particles from the air.
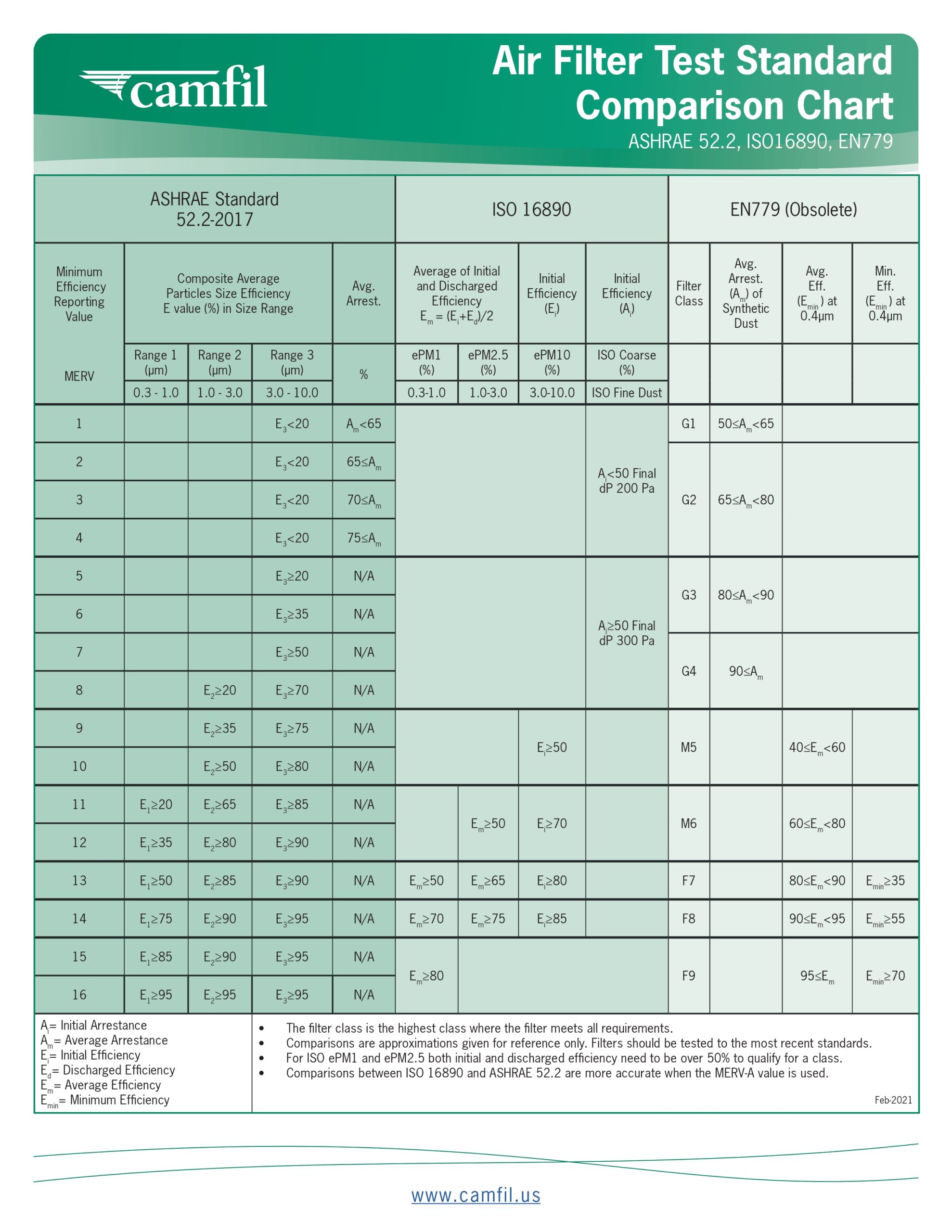 ASHRAE recommends using MERV 16-rated filters in common hospital spaces like Class 3 imaging, cesarean delivery and general surgery operating rooms. These filters are known for their ability to capture tiny droplet nuclei (like those from sneezes) and bacteria. However, these filtering recommendations may not be sufficiently effective in rooms occupied by patients with infectious diseases.
ASHRAE recommends using MERV 16-rated filters in common hospital spaces like Class 3 imaging, cesarean delivery and general surgery operating rooms. These filters are known for their ability to capture tiny droplet nuclei (like those from sneezes) and bacteria. However, these filtering recommendations may not be sufficiently effective in rooms occupied by patients with infectious diseases.
HEPA Filters Work with Other Filters
HEPA filters are a key component in controlling air quality within AIIRs. They come in various forms. For example, global air filtration specialist Camfil offers HEPA air filter panels for terminal filtration in panel configurations and box-type HEPA filters which are often installed as the final stage of filtration in HVAC systems. tAir filters with lower efficiency are installed in the stages prior to HEPA filters to enhance overall efficiency and to lessen the burden on the main HEPA filter, thereby extending its useful life.
For instance, air-handling units in isolation rooms might use a MERV 14 pre-filter paired with a HEPA filter to capture the finest particles. Pre-filters, like the Hi-Flo ES a high efficiency bag filter, capture larger particles before they reach the main HEPA filter, helping to maintain the integrity and extend the lifespan of the more costly HEPA filters. These pre-filters, which are efficient in energy use due to their low-pressure drop, can be rated from MERV 11 to MERV 15.
In situations where space is limited, the Camfil Durafil ES high-performance V-bank air filters are used as pre-filters to the main HEPA filter. These are available in MERV 13 to MERV 16 ratings, ensuring that even in compact air handling units, filtration is not compromised.
Maintaining Filter Efficiency
To ensure that AIIR rooms function effectively, it’s essential to maintain the filtration system properly, even with a top-tier HVAC system in place. This means that filters should be serviced or replaced regularly for the best performance. Indicators that a filter needs replacing include:
- Decreased airflow that relates to less efficiency in capturing particlesExcess accumulation of dust and particulates within the space being protected
- Increased power consumption as the HVAC system works harder to pump air through a clogged filter
- Gaps in and around filter banks causing particles to bypass filter fibers
In addition, it’s crucial to follow the filter replacement schedule provided by the manufacturer, regardless of whether the above signs are present.
Improving Hospital Safety Records
The COVID-19 pandemic highlighted the necessity of effective isolation methods within healthcare facilities to curb the spread of infectious diseases. AIIRs are critical in this effort, as they isolate patients with contagious diseases and prevent the spread of airborne pathogens within the hospital.
Proper ventilation is also crucial to halt the spread of diseases transmitted via airborne particles. Implementing a top-tier air filtration system is a sound investment, preventing expensive and potentially deadly outbreaks. This is particularly important for the elderly and other patients with weakened immune systems. Infectious disease containment is a measure of a hospital’s commitment to safety, influencing its reputation and standing in the community.
HEPA filters are vital in isolation rooms, with medical-grade HEPA filters outperforming other types by removing 99.9% of particles as small as 0.3 µm. Although less efficient filters can be used effectively as prefilters, HEPA filters are the cornerstone for eradicating airborne pathogens from an AIIR.
The selection of HEPA filters depends on various factors, including the size of the facility, contamination levels, budget constraints, industry standards, and maintenance costs.
Consulting with an air filtration expert, particularly one with healthcare industry experience like Camfil, can help a hospital determine the appropriate medical-grade HEPA filter for any AIIR. Camfil trained experts can advise on how to design a system of staged filters that will best prevent the transmission of infectious agents.
¹Transmission-Based Precautions, Centers for Disease Control, Transmission-Based Precautions | Basics | Infection Control | CDC”
²Al-Benna, Sammy; van Zijl, Francie. The Association for Perioperative Practice. December 1, 2020. Sage Journals. Negative pressure rooms and COVID-19 – Sammy Al-Benna, 2021 (sagepub.com)
³Andersen, Bjorg Marit. Prevention and control of Infections in Hospitals. Background Information, Isolation Routines. September 25, 2018. National Library of Medicine. Background Information: Isolation Routines – PMC (nih.gov)
⁴Bannister, Barbara; Puro, Vincenzo, Fusco; Francesco, Heptonstall; Julia, Ippolito; Giuseppe. Framework for the design and operation of high-level isolation units: consensus of the European Network of Infectious Diseases. National Library of Medicine. Framework for the design and operation of high-level isolation units: consensus of the European Network of Infectious Diseases – PMC (nih.gov)
⁵Herstein, Jocelyn; Iwen, Peter; Jelden, Katelyn; Biddinger, Paul: Gibbs, Shawn: Le, Aurora: Hewlett, Angela: Lowe, John. U.S. High-Level Isolation Unit Clinical Laboratory Capabilities Update. National Library of Medicine. U.S. High-Level Isolation Unit Clinical Laboratory Capabilities Update – PMC (nih.gov)
⁶Guidelines for Environmental Infection Control in Health-Care Facilities. Background C. Air. 2003. Centers for Disease Control and Prevention. https://www.cdc.gov/infectioncontrol/guidelines/environmental/background/air.html
⁷Types of Airborne Disease, Healthline, https://www.healthline.com/health/airborne-diseases#types
⁸Ventilation of Heal Care Facilities, ANSI/ASHRAE/ASHE addendum to ANSI/ASHRAE/ASHE Standard 170-2017. ANSI/ASHRAE/ASHE Addendum s to ANSI/ASHRAE/ASHE Standard 170-2017
⁹Isolation Rooms. International Health Facility Guidelines. https://healthfacilityguidelines.com/ViewPDF/ViewIndexPDF/iHFG_part_d_isolation_rooms
¹⁰Ventilation in Buildings, Centers for Disease Control and Prevention. May 12, 2023. https://www.cdc.gov/coronavirus/2019-ncov/community/ventilation.html
¹¹Hospital Isolation Room Requirements – What You Need to Know. Thomas, a Xometry Company. https://www.thomasnet.com/articles/plant-facility-equipment/hospital-isolation-room-requirements/
¹²Ventilation of Heal Care Facilities, ANSI/ASHRAE/ASHE addendum to ANSI/ASHRAE/ASHE Standard 170-2017. ANSI/ASHRAE/ASHE Addendum s to ANSI/ASHRAE/ASHE Standard 170-2017